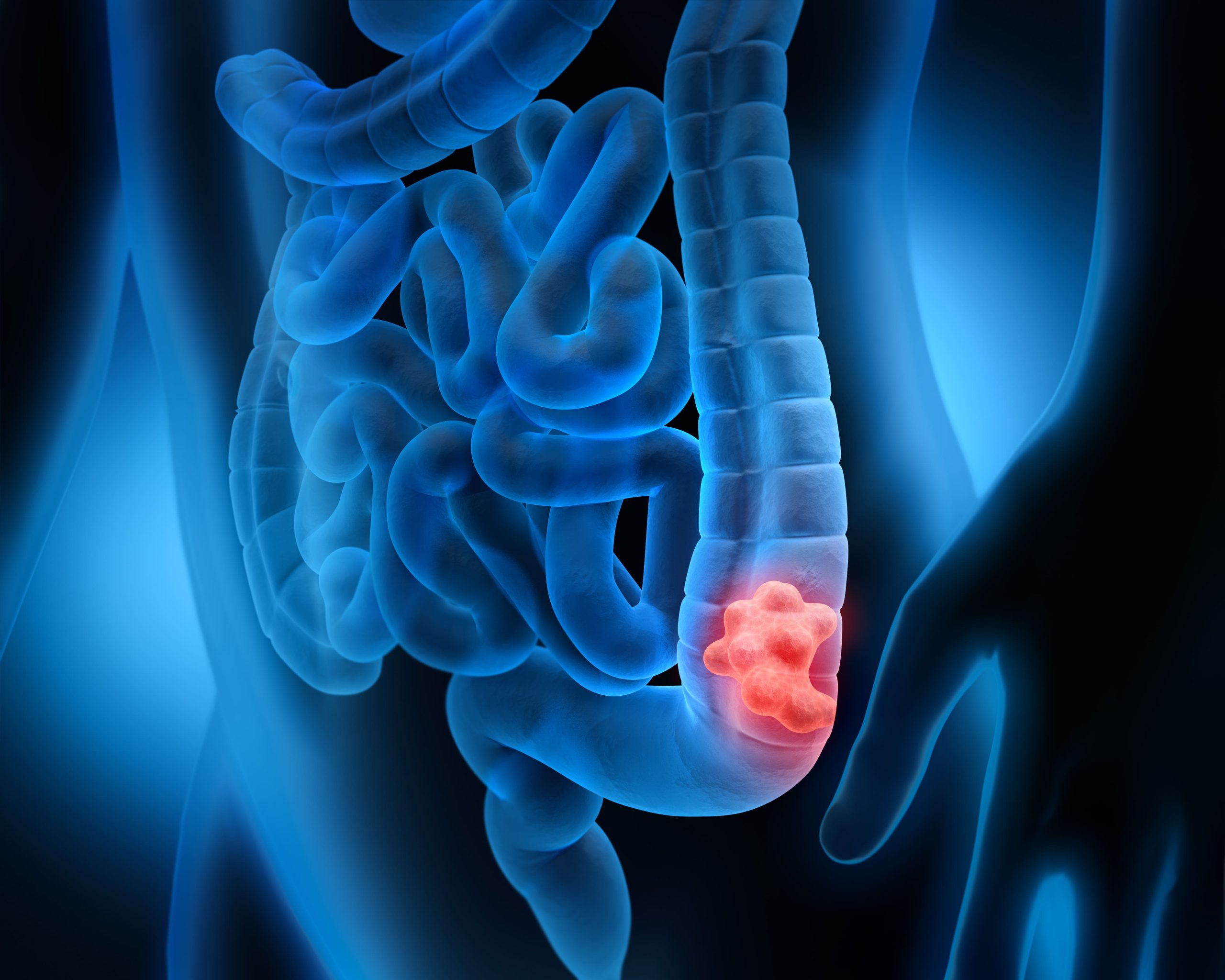
In recent years, a concerning trend has emerged that has captured the attention of the global medical community: a rising number of young adults are being diagnosed with colon cancer, a disease historically associated with older age. This unexpected shift raises significant questions about its causes and presents challenges for early detection and treatment.

Colon Cancer Among Young Adults: A Growing Concern
Traditionally seen in older populations, colorectal cancer is now increasingly affecting young adults. Studies reveal a consistent rise in early-onset cases globally, with some countries experiencing sharp increases. In England, bowel cancer cases among individuals aged 25 to 49 have risen by 3.6% annually over the past decade, as reported in The Lancet Oncology. Similarly, data from 50 countries show escalating rates in younger adults across 27 nations, including high-income countries like the U.S., Australia, and Canada.
In the United States, the American Cancer Society (ACS) noted that colorectal cancer diagnoses in those under 55 nearly doubled from 11% in 1995 to 20% in 2019. For 2024, the ACS projects approximately 19,550 cases and 3,750 deaths among individuals under 50. Distressingly, colorectal cancer has become the second leading cause of cancer-related deaths among women under 50 and the leading cause for men in the same age group.
Certain populations are more affected by these trends. In the U.S., Black men and women have historically faced higher incidence and mortality rates, prompting earlier screening recommendations. However, sharp increases are now also observed among White individuals, particularly in rural or underserved areas. Globally, countries experiencing lifestyle changes—marked by higher consumption of processed foods and sedentary habits—are witnessing similar spikes.
Late Diagnoses and Challenges
Most young adults diagnosed with colorectal cancer are already at advanced stages—Stage III or IV—where treatment is more complex. This is due to a lack of routine screenings for those under 45 and the misattribution of symptoms to less serious conditions like hemorrhoids or irritable bowel syndrome (IBS).
These troubling statistics underscore the need for heightened awareness and earlier interventions. Recently, the U.S. Preventive Services Task Force lowered the recommended screening age from 50 to 45 for average-risk individuals, acknowledging the demographic shift in colorectal cancer cases.
Dr. Phil Daschner of the National Cancer Institute noted, “We don’t understand a lot about the causes, the biology, or how to prevent early onset of the disease. And that’s important to learn more about because it may affect [approaches for] the treatment and survivorship of early-onset colon cancer.”
Investigating Potential Causes
The reasons behind this increase in early-onset colon cancer remain unclear, but several factors are believed to contribute:
Lifestyle and Diet:
Modern dietary habits, including high consumption of processed meats and fats with low intake of fruits and vegetables, are strongly linked to colon cancer. The Western diet, characterized by its high-calorie, low-nutrient profile, can contribute to obesity and gut microbiome imbalances, increasing cancer risk. Sedentary lifestyles further exacerbate the issue, as prolonged inactivity is associated with higher cancer rates.
Environmental Exposure:
Chemical exposure, including endocrine disruptors and obesogens, may also play a role. Persistent environmental chemicals can interfere with hormonal and metabolic processes, contributing to obesity and potentially increasing cancer risk. The National Institute of Environmental Health Sciences has identified several substances that could influence gut health or DNA integrity, fostering cancer development.

Gut Health and Inflammation:
An unhealthy gut microbiome may promote chronic inflammation, damaging DNA and encouraging tumor growth. Conditions like Crohn’s disease, IBS, and diabetes, which are associated with chronic gut inflammation, further heighten the risk of colon cancer.
Genetic and Epigenetic Factors:
Family history and genetic predispositions remain significant risk factors. Additionally, environmental factors interacting with individual genetics and epigenetics add complexity to understanding the disease’s origins.

Recognizing Symptoms
Early detection is critical to improving outcomes. Symptoms of colorectal cancer to watch for include:
- Rectal Bleeding: Blood in stool or on toilet paper, reported by nearly half of young patients.
- Abdominal Pain: Persistent discomfort, particularly in the lower abdomen.
- Changes in Bowel Habits: Prolonged constipation, diarrhea, or narrow stools.
- Unexplained Weight Loss and Fatigue: Sudden weight loss or severe tiredness alongside other symptoms.
Since younger patients often appear healthy and may not exhibit symptoms initially, consistent vigilance is crucial. Persistent symptoms should prompt immediate medical attention.

Prevention and Risk Reduction
Reducing colorectal cancer risk involves adopting healthier lifestyles and prioritizing screenings:
- Maintain a healthy weight.
- Engage in regular physical activity.
- Follow a fiber-rich diet with fruits, vegetables, and whole grains.
- Limit red and processed meat consumption.
- Moderate alcohol intake and avoid tobacco use.
- Participate in regular screenings, starting at age 45 or earlier for high-risk individuals.
Raising Awareness
The rise in colorectal cancer among young adults calls for collective action to address its causes and improve early detection. By embracing healthier habits, staying informed about risks, and supporting public health initiatives, we can combat this concerning trend.
Although challenging, colorectal cancer is a battle that can be fought through vigilance and informed action. Early recognition of symptoms, understanding personal risks, and fostering awareness are critical steps in reversing this troubling increase among younger populations.

